In today's diverse healthcare landscape, cultural competency is crucial, especially at centers like Kaiser Permanente Mental Health Access Center in Northglenn. This involves providers recognizing and respecting patient cultural beliefs, improving trust and relationships, particularly for sensitive mental health issues. Effective community outreach programs enhance overall health outcomes. Training focused on cultural sensitivity helps bridge the gap for underrepresented groups that mistrust traditional healthcare systems, leading to better communication, treatment engagement, and mental health outcomes. Kaiser Permanente Northglenn innovates with tailored initiatives, revolutionizing care access and understanding for diverse communities. Comprehensive training, including role-playing, case studies, and coaching programs, ensures personalized care based on cultural beliefs, resulting in improved patient outcomes.
In today’s diverse healthcare landscape, cultural competency is no longer an option but a necessity. Understanding and respecting patients’ cultural backgrounds and beliefs significantly impacts healthcare outcomes, especially in mental health care. This article explores the critical role of cultural competency training for healthcare providers. We delve into successful programs like the Kaiser Permanente Northglenn Mental Health Access Center, showcasing innovative approaches that enhance patient access and outcomes. Key strategies for effective training are also discussed.
- Understanding Cultural Competency in Healthcare: A Necessity in Modern Medicine
- The Impact of Cultural Competence on Mental Health Care Access
- Kaiser Permanente Northglenn: A Center for Innovative Training Programs
- Strategies for Effective Cultural Competency Training in Healthcare Settings
- Enhancing Patient Outcomes: Real-World Success Stories from the Kaiser Permanente Model
Understanding Cultural Competency in Healthcare: A Necessity in Modern Medicine
In modern healthcare, understanding cultural competency is no longer an option but a necessity. This concept involves recognizing and respecting diverse cultural beliefs, values, and practices within patient populations. With communities becoming increasingly diverse, healthcare providers must be equipped to deliver culturally sensitive care that addresses the unique needs of every individual. At centers like Kaiser Permanente Mental Health Access Center in Northglenn, this approach is pivotal in ensuring equitable access to quality mental health services.
Cultural competency goes beyond simple awareness; it empowers healthcare professionals to adapt their practices and communication styles. This is especially crucial when addressing sensitive issues like emotional regulation and mood management, where cultural nuances can significantly impact patient engagement and treatment outcomes. Effective implementation of community outreach programs that promote this competency can foster trust, enhance patient-provider relationships, and ultimately improve overall health outcomes in diverse communities.
The Impact of Cultural Competence on Mental Health Care Access
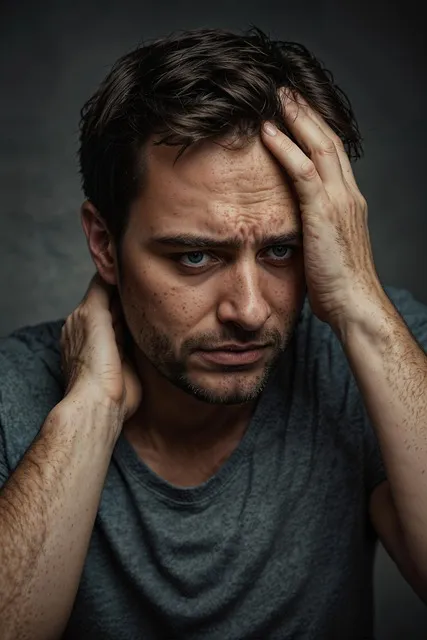
Cultural competence plays a pivotal role in ensuring equitable access to mental health care services. In communities with diverse cultural backgrounds, such as those served by the Kaiser Permanente Mental Health Access Center in Northglenn, addressing cultural barriers is essential to improving healthcare outcomes. Many individuals from underrepresented groups face challenges in accessing mental health support due to historical and systemic issues that create mistrust and apprehension towards traditional healthcare systems.
Training programs focused on cultural sensitivity in mental healthcare practice equip providers with the skills to offer empathetic, culturally tailored care. By learning effective conflict resolution techniques, healthcare professionals can foster stronger relationships with patients from different cultural backgrounds, encouraging open communication and understanding. This approach not only enhances the emotional healing processes for patients but also promotes better engagement and adherence to treatment plans, ultimately improving mental health outcomes in diverse communities.
Kaiser Permanente Northglenn: A Center for Innovative Training Programs
Kaiser Permanente Northglenn stands as a beacon for innovative healthcare training programs, focusing on cultural competency and mental health access. This center has pioneered unique initiatives aimed at bridging the gap between diverse communities and quality mental wellness services. Through its comprehensive approach, Kaiser Permanente Northglenn offers not just training but also resources like Mental Wellness Journaling Exercise Guidance, designed to empower providers and patients alike.
The facility’s commitment extends beyond traditional training methodologies, incorporating Mental Illness Stigma Reduction Efforts and Public Awareness Campaigns Development. These initiatives reflect a holistic strategy to foster an inclusive environment where every individual feels comfortable seeking mental health support. By combining cutting-edge training with public engagement, Kaiser Permanente Northglenn is revolutionizing healthcare delivery, ensuring that mental wellness is accessible and understood across diverse cultural landscapes.
Strategies for Effective Cultural Competency Training in Healthcare Settings

Effective cultural competency training in healthcare settings involves a multi-faceted approach tailored to address the diverse needs of patients and communities. At the Kaiser Permanente Mental Health Access Center Northglenn, for instance, programs are designed to foster understanding and empathy among healthcare providers. This includes exposing staff to various cultural perspectives through role-playing scenarios, case studies, and workshops that simulate real-life interactions with patients from different backgrounds. By engaging in these activities, providers can enhance their communication strategies, building resilience in handling sensitive topics related to mental wellness.
Moreover, integrating Mental Wellness Coaching Programs into the training curriculum equips healthcare professionals with tools to navigate cultural nuances effectively. These programs emphasize active listening, culturally sensitive questioning, and adaptive communication techniques. Through regular practice, staff gain confidence in addressing mental health concerns while respecting individual cultural beliefs and practices. This holistic development ensures that patients from diverse communities receive personalized care that considers their unique needs and promotes positive mental wellness outcomes.
Enhancing Patient Outcomes: Real-World Success Stories from the Kaiser Permanente Model

Healthcare provider cultural competency training plays a pivotal role in enhancing patient outcomes, especially within diverse communities. A notable success story comes from Kaiser Permanente’s Mental Health Access Center in Northglenn, Colorado. This center has demonstrated that by integrating Mind Over Matter Principles into their practices, they’ve significantly improved access to mental health services and reduced instances of Depression Prevention among patients from various cultural backgrounds.
The center’s approach involves not just treating symptoms but also focusing on Self-Awareness Exercises tailored to individual cultures. Through this holistic method, providers foster a deeper understanding of their patients’ unique perspectives and needs, leading to more effective care. The Kaiser Permanente model serves as a testament to how cultural competency training can revolutionize healthcare delivery, ensuring better outcomes for all.
Cultural competency training is no longer a nice-to-have in healthcare—it’s an essential tool for improving patient outcomes, particularly within mental health care. As evidenced by Kaiser Permanente’s successful programs at their Northglenn Mental Health Access Center, innovative training models can foster understanding and improve access to care for diverse populations. By integrating these strategies into healthcare settings, we can move towards a more inclusive and effective system that prioritizes the well-being of all patients, regardless of cultural background.